We work closely with a network of specialized professionals to deliver comprehensive care. Our providers are experts in their fields, offering innovative solutions tailored to your needs.
Working with World Class Scientists and Specialist Physicians in London Ontario, we help get you back to doing the things that make life worth living.
Comprehensive testing includes videonystagmography (VNG), rotational chair tests and tests for balance and verticality.
What is the vestibular system, and what role does it play in our daily lives?
The vestibular system is a sensory system located within the inner ear (peripheral). It plays a critical role in helping us maintain balance, posture, and coordination. It provides real-time feedback to the brain about head position and motion, allowing us to move smoothly through space without feeling dizzy or disoriented (central).
How does the vestibular system help us maintain balance (central)?
The vestibular system detects changes in head movement and position, sending signals to the eyes and muscles to stabilize vision and control posture. It works closely with the visual and proprioceptive systems to keep us upright and oriented.
Can you describe the main parts of the vestibular system and their functions?
The vestibular system includes the semicircular canals (which detect rotational movement), the otolith organs—the utricle and saccule (which detect linear acceleration and gravity), and the vestibular nerve that sends signals to the brain. These components work together to interpret head movements and spatial orientation.
How do the inner ear structures contribute to our sense of balance?
The semicircular canals respond to head rotation, while the otoliths detect up-down or side-to-side motion. Hair cells in these structures convert mechanical movement into nerve signals, informing the brain about how we are moving relative to gravity and space. (Processed via central).
What are some common disorders or issues related to the peripheral and central vestibular system?
The vestibular system includes the semicircular canals (which detect rotational movement), the otolith organs—the utricle and saccule (which detect linear acceleration and gravity), and the vestibular nerve that sends signals to the brain. These components work together to interpret head movements and spatial orientation.
Common disorders include:
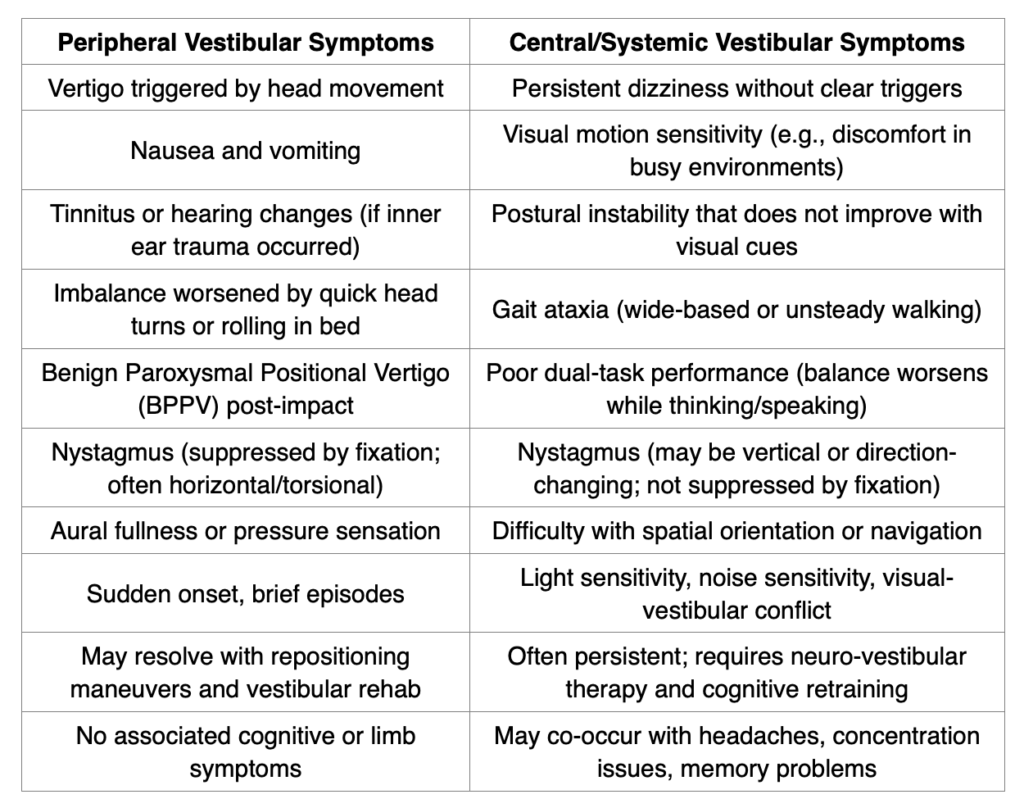
How can patients recognize the symptoms of vestibular system disorders?
Key symptoms include:
Vestibular Symptoms After Acquired Brain Injury (mild/moderate/traumatic and mTBI)
(Based on neuro-otologic and vestibular rehabilitation literature)
Sources:
What are the typical steps involved in diagnosing a vestibular disorder?
A diagnosis begins with a detailed history and symptom review, followed by a series of objective tests to measure vestibular function. We examine eye movements, balance, and responses to specific stimuli.
What kinds of tests or examinations might a patient undergo?
Your treating physician may order:
Each test evaluates different parts of the vestibular system.
*Not all tests are needed for all patients. Please consult your provider.
Otology/Neurotology recommendations – Choosing Wisely campaign
What are the common treatments available for vestibular disorders?
Treatment depends on the diagnosis and may include:
Can lifestyle changes or exercises help manage or improve vestibular health?
Absolutely. Regular physical activity, hydration, stress reduction, and avoiding vestibular/migraine triggers (such as caffeine or certain lighting) can significantly help. Vestibular physiotherapy exercises are often prescribed to retrain the brain and improve balance.
What should patients expect during a vestibular assessment?
Expect a thorough and gentle process. Patients will sit or stand for various tests that monitor eye movements, head movements and balance. Most tests are non-invasive and well tolerated.
As it is a third-party claim (auto/life/disability/WSIB), legal representative or adjuster/adjudicator may also recommend testing.
How can patients best prepare for their appointments?
Wear comfortable clothing, avoid makeup around the eyes, bring list of medications and symptoms (this is also done previously through self-assessment). It is helpful to avoid alcohol or sedating medications 24 hours prior.
What are some of the latest advancements in the treatment and diagnosis of vestibular disorders?
Advances include:
How is technology being used to improve patient outcomes?
We use objective data from high-tech equipment to create individualized treatment plans. Technology enhances precision, which leads to better, faster recovery.
Are there any preventative measures to maintain a healthy vestibular system?
Yes—staying physically active, minimizing head trauma, treating infections promptly, and avoiding ototoxic medications, when possible, all contribute to vestibular health.
How does overall health impact vestibular function?
Strong cardiovascular health, proper hydration, and mental wellness all support optimal vestibular function. Stress and poor sleep can exacerbate symptoms, so holistic health matters.
I am having trouble focusing. My MD said my eyes lag behind my head. What does that mean?
This refers to a dysfunction in the vestibulo-ocular reflex (VOR)—the reflex that stabilizes vision during head movement. If your eyes do not move in sync with your head, visual clarity suffers. Further vestibular testing is advised.
Should I get better testing?
Your doctor may recommend a full vestibular assessment with specialized equipment can pinpoint the issue and guide effective treatment.
What does it mean if I feel nauseated when my eyes open and close and I feel like I am spinning?
That is a classic vertigo symptom, peripheral or central. It can be evaluated with positional tests and objective diagnostics.
How does something like this get tested?
We use tools like VNG, rotary chair, and vHIT to measure eye and balance responses under different conditions, even with eyes closed, to determine the root cause.
What is the difference between a caloric test and a vHIT?
Caloric Test: Stimulates each ear individually using warm and cool air or water to provoke a response. It assesses low-frequency function of the horizontal semicircular canal. By design can miss lesion that will show on vHIT.
vHIT (Video Head Impulse Test): Measures high-frequency head movement responses across all six canals in real time using high-speed cameras.
How do your reports help the physiotherapist?
Our reports include objective data on each vestibular structure's function. This guides physiotherapists to create targeted rehab plans, improving patient recovery efficiency and outcomes.
Is rotary chair testing considered a “novel” science?
No. Rotary chair testing is an established, gold-standard method for assessing the vestibulo-ocular reflex. It offers precise, reproducible data and is recognized internationally in academic and clinical settings.
While ENT and Neurotology are key players, vestibular care is highly interdisciplinary.
Other health professionals involved include:

A vestibular assessment identifies how your balance system is functioning. It helps diagnose the root cause of symptoms like dizziness or imbalances supporting both effective treatment and medical necessity for insurance claims.
By pinpointing which parts of your balance system are affected, we can create targeted treatment plans. This speeds recovery and makes it easier to return to work with improved focus, balance, and movement tolerance.
With your consent, we provide timely updates—ranging from full clinical reports to brief summaries—so your care team stays informed and aligned throughout your rehab journey.
Yes. Our team can determine if symptoms are vestibular in origin or related to other conditions like concussion or anxiety. We assess eye movement, balance, and overall function to guide accurate treatment.
We believe education is key. From day one, you’ll understand your symptoms and treatment options. This knowledge empowers you to take control and actively participate in your recovery.

A vestibular assessment offers objective proof of balance issues, often caused by concussions or injuries. This medical evidence strengthens your claim, supports treatment plans, speeds up processing, and helps demonstrate the real impact on daily life.
Because hearing and balance share the inner ear, combining assessments gives a full picture of what is wrong. This leads to better diagnosis, clearer understanding of symptoms, and more effective, personalized treatment plans.
Reports provide clear, objective evidence of inner ear dysfunction. When paired with audiology results, they help case managers, lawyers, and insurers understand your condition and support your claim with credible, easy-to-understand data.
Together, they uncover hidden symptoms, explain post-injury struggles, and build stronger medical evidence. This combined approach ensures accurate diagnosis and targeted recovery plans after car accidents, workplace injuries, or concussions.
By working as a team, they explain results clearly, offer tailored recovery plans, track progress, and provide consistent support. Patients feel informed, encouraged, and actively involved in their healing journey.